Dr Nathaniel-Edouard Davidson, Associate Member of the College and winner of the inaugural CGDent-GC Award, reflects on what he learnt at the first Introduction to Occlusion Symposium and why you should go to the next one.

When I first saw the announcement for the Introduction to Occlusion Symposium, I was not sure if it was for me. Occlusion felt like one of those important, yet complex (and slightly intimidating) areas of dentistry where it’s difficult to apply the extensive teachings in day-to-day practice. However, after dealing with a rising number of fractured restorations, TMJ complaints, and patients reporting muscle soreness and headaches, I realised I needed to deepen my understanding.
From the moment the first lecture started, it was clear this was not just a day of theory. The symposium tackled real-world challenges that many of us face every day in practice. The sessions covered everything from the history and implications of occlusal disease to practical techniques for restoring worn dentitions; always maintaining a strong focus on understanding the “why” behind the “what.”

The first Introduction to Occlusion Symposium in London, 5 April 2025
What stood out most
One of the key points from the day was to focus on the high prevalence of occlusal disease, which is even more common than caries or periodontal disease. There are many signs that indicate the presence of occlusal disease, such as fractured cusps, worn-down restorations, mobility, gingival recession, abfraction lesions, TMJ pain, headaches. These issues often seem unrelated, however, the symposium effectively demonstrated how these issues are in fact interconnected.
“A single night of bruxism can cause as much damage as a lifetime of chewing”. This significant insight was discussed, along with how the loss of proprioception during sleep can result in forces generated by nocturnal clenching increasing tenfold. This may explain the rise in failed restorations and unexplained wear.
Practical knowledge I’m already applying
One of the best aspects of the symposium was the clear, actionable treatment planning advice. We discussed the importance of the “Five Laws” for an ideal occlusion and successful occlusal appliance:
- Mutually protected occlusion
- RCP = ICP around the retruded axis position
- Anterior guidance
- No non-working side interferences
- Posterior stability
Frameworks like these make managing occlusion more straightforward.
We also explored how to manage occlusal wear with restorative approaches. One fascinating technique that stood out was the use of additive composite canine risers. We can maintain the intercuspal position, but through the use of composite additions to the canines we can reintroduce anterior guidance – this alone can disclude posterior teeth and prevent further wear. It’s simple, it’s effective, and it’s something I can do in day-to-day practice.
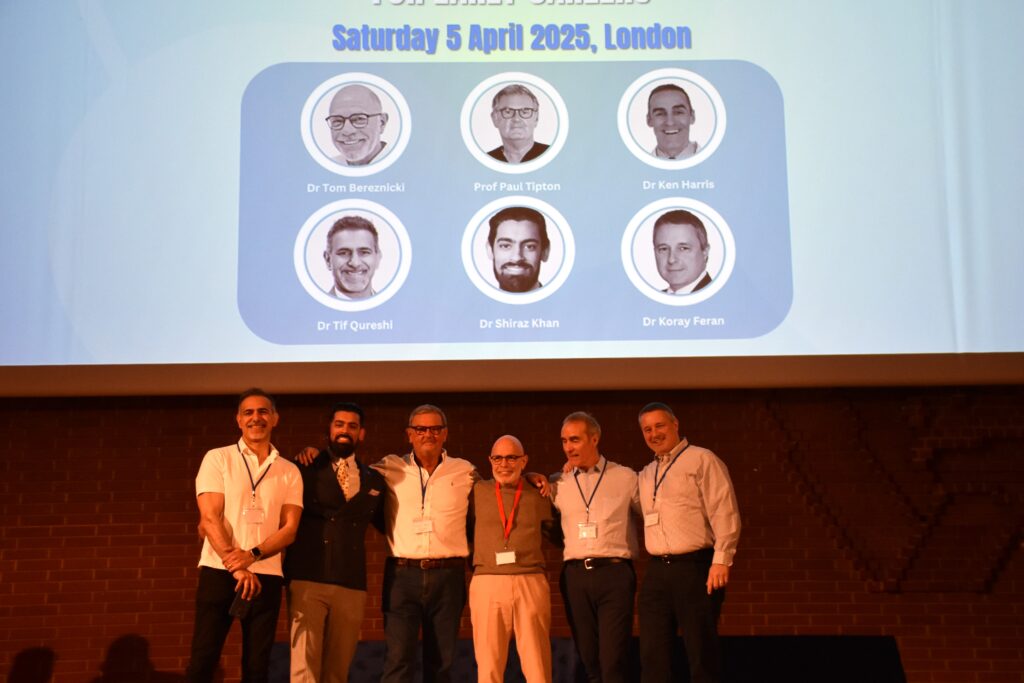
The Introduction to Occlusion Symposium speakers (l-r): Dr Tif Qureshi FCGDent, Dr Shiraz Khan, Professor Paul Tipton FCGDent, Dr Tom Bereznicki FCGDent, Dr Ken Harris FCGDent and Dr Koray Feran FCGDent
A shift in perspective
The symposium clarified occlusion terminology, particularly centric relation (RCP) versus intercuspal position (ICP). I now understand that while ICP is used for day-to-day dentistry, centric relation is stable and reproducible for complex treatments. Knowing when to use each position and whether to conform or reorganise has improved my approach.
The rule of thumb we learnt
Reorganise: when there is heavy wear, multiple restorations, TMJ symptoms, or a need to increase vertical dimension.
Conform: when the five laws of ideal occlusion (as mentioned above) are met, when there are fewer restorations to carry out, or when there are potential financial constraints.
What I’ll do differently now
Since attending the symposium, I have already started using articulating paper markings in both RCP and ICP and taking intraoral photos and scans to help with diagnosing current or potential future occlusal problems. I am more able to practically ‘see’ a reduced envelope of function. Patients who used to report “chipping front teeth” now make me think of reduced overbite and a collapsed envelope of function, rather than just failing restorations and parafunctional habits.
In addition, I am now more proactive about spotting early signs of parafunction, reducing interferences and offering occlusal splints. Perhaps most importantly, I now understand that restoring anterior guidance early might actually save the need for more invasive posterior restorations later. The symposium has motivated me to pursue further learning and has provided clear direction on where to focus my efforts.
Why should you attend the Occlusion Symposium?
This symposium did more than just teach occlusion – it sparked a genuine interest in the subject and gave me practical tools I can use right away. It is easy to overlook occlusion in favour of more popular topics in dentistry, but this symposium reinforces that getting the fundamentals right is what leads to predictable and long-lasting results.
If you are on the fence about attending a future occlusion symposium, I would say this: do it. Whether you are early in your career or years into practice, the insights you will gain are invaluable. If you are a Principal of a practice, why not encourage your Associates to attend? It is not just about protecting teeth, it is about treating the whole system, understanding function, and elevating the quality of care you can provide.

The next Introduction to Occlusion Symposium will take place in Edinburgh on Saturday 1 November 2025. Open to all dental professionals and with six hours’ CPD, tickets are just £90 for those who qualified between 2020 and 2025, and £110 for all other attendees. For further information, and to book your place, visit our event page