In his recent CPD seminar, delivered for the College at Dentistry Show London, Jason Wong MBE FCGDent, Deputy Chief Dental Officer for England, discussed contemporary concepts relating to patient safety, and in this blog, examines recent developments.

For some years I have spoken about the culture of fear and anxiety that has gripped the dental profession in the United Kingdom and how it has wide ranging impacts including its effect on the culture in clinical practice, limiting access to care and wellbeing of the dental workforce.
In a nutshell, what I was asked to speak about by the College of general Dentistry at the recent Dentistry show London, is how we, the dental profession, are attempting to initiate steps to move away from the current blame and fear culture to a fair and learning culture, and how this will improve patient safety.
I have always had an interest in this area, and from my time as a Local Dental Network Chair in the Midlands, and with my Leadership fellow Dr Priya Chohan and Oral Surgeons Professor Tara Renton and Dr Edmund Bailey, published an article in the British Dental Journal which concluded that there is a lack of knowledge concerning Patient Safety Incident reporting and a culture of fear affecting the profession.
Coincidentally, one of the first things I was asked to work on when I was appointed as Deputy Chief Dental Officer for England was whether wrong tooth extraction should still be classed as a Never Event by the NHS.
On 17 June 2021, I brought together key stakeholders from across dentistry to discuss the significant potential for patient safety improvement. The group’s discussions concluded with a commitment to work together in collaboration with the profession, to better embed a culture of fairness, openness and learning with regards to patient safety in dental settings.
At the core, we knew that we needed to address the issue of what to record and what to report. We have looked at the available literature and have concluded that barriers to recording and reporting patient safety issues in dentistry is not just an England problem or even a UK problem, but a worldwide one.
At the same time, we welcomed the introduction of the Learn from patient safety events (LFPSE) service, which will support patient safety improvement across all dental care settings. We are encouraging recording of Patient Safety Events but there is still some work to align the system so that it is more user-friendly for dental practices.
Using LFPSE to record and share details of Patient Safety Events means that we could be participating in a profession-wide effort to support national safety improvement work. We recognise that most dental care is delivered in safe settings by caring practitioners, and that the profession has a safety record of which it can be proud.
However, there is always more to be done to ensure that we are delivering the best possible care for patients. Whilst event reporting is a vital tool for information gathering, patient safety engagement, and shared learning, further work is needed to facilitate a just culture for patient safety in dental settings.
Maintaining consistent, constructive, and fair evaluation of Patient Safety Events will facilitate a supportive and safe learning environment for all colleagues. Consistent evaluation will also aid local safety improvements, while assisting continuing professional development and encouraging personal reflection.
It has been a major advantage to align our work with the rest of primary care and the NHS Patient Safety Strategy, so that dentistry does not work in a silo. We therefore have NHS officials attend our meetings and we attend their strategy meetings, and the work that our group has carried out has been well received by the NHS.
However, defensive dentistry is rife, a lack of clarity about what is best and acceptable practice means that there is significant cognitive dissonance alongside the anxiety and fear.
What is patient safety?
Patient safety is the avoidance of unintended or unexpected harm to people during the provision of health care. We support providers to minimise patient safety incidents and drive improvements in safety and quality. Patients should be treated in a safe environment and protected from avoidable harm.
In the CGDent/Dentistry Show London presentation, I examined the principles contained in official publications, several well-known books as well as the patient safety syllabus from HEE’s e-Learning for Healthcare (e-LfH) programme.
Project Sphere
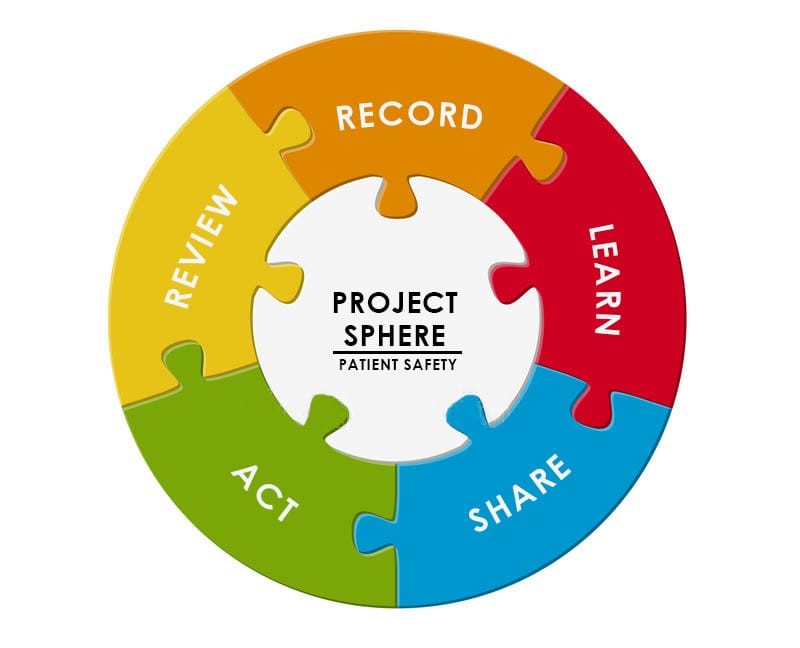
Regional HEE Clinical Leadership Fellow and Dental Therapist, Jyoti Sumel, also presented at the Dentistry Show London this year. Jyoti leads Project Sphere, a project aimed at improving patient safety recording. The Project Sphere working group wants to initiate a culture change, a change that will see dental care move from a perceived blame culture to a learning culture.
They are encouraging the entire dental team to get involved: the safety of patients requires a team approach and is the responsibility of every individual. Project Sphere currently has wide ranging aims to improve systems for learning, recording and workforce support.
The Project Sphere group is fortunate to have both support for their work from both regulators and indemnity. With their support there is a real opportunity to affect the change they want to make.
Clinical leadership
Recent studies of organisational culture and patient safety emphasise the role of senior leadership. Senior leaders can support learning and communicate the importance of safety over other organisational goals. Effective leaders show active engagement with patients and staff and this has a bearing on safer patient care.
Dentists, dental nurses, and dental care professionals can all play an important part as clinical leaders. Clinical leaders make sense of patient safety problems, mobilise resources and put solutions in place. They also create a just culture which encourages colleagues to speak up when things go wrong, rather than fearing blame.
So how do you start to cultivate these principles in your practice?
Here are my top ten tips:
Leadership
- Be genuine and build a vision for the whole practice
- Be a genuine learning practice
- Create a safe working environment
- Build relationships – show genuine concern for interests of co-workers and patients
- Lead by example
Communication culture
- Optimal communications – try using freely available digital platforms to improve communication
- Help to make traditions
- Celebrate wins
- Clear job description & expectations – identify strengths
System culture
- Continue to develop comprehensive systems tailored to your setting
Have fun if possible but do build a system that everyone can work to.
Project Sphere – the future
Project Sphere will continue its work this coming year and will continue to socialise the concepts that I have been discussing in this blog. The College of General Dentistry has kindly agreed to publish some guidance for the workstream, the first of which involves lone working and the circumstances that surround it in dental settings. The Project Sphere group are working with the indemnity providers on a consensus statement to reassure clinicians, as well as guiding them to the best place to obtain advice. Hopefully the early positive signs from the impact of their work will continue to develop. As for culture change, that will take some time but the journey has to start somewhere and we hope that this will be the start of many positive changes in dentistry.
Free webinar for all dental professionals
Dental professionals are invited to join a free webinar to learn more about creating a positive patient safety culture, with Jason Wong. The webinar, Creating a positive patient safety culture in dentistry, takes place at 7pm on Tuesday 10 January 2023.
The webinar, hosted by the College and available through ProDental CPD, is free to view live for all dental professionals, but prior registration is required. College members will have free access to the recording afterwards.

