Sana Masood, third-year dental student at the University of Bristol, uncovers some of the more surprising things she has learnt at dental school.

Dental school is a place of academic rigor, long hours, and plenty of theoretical learning. But in between the lectures, exams, and clinical work, dental students often pick up some unexpected lessons that become just as vital to their success as anything they’ve been taught in class. From the art of patient communication to mastering the fine line between precision and creativity, here are some of the more playful, yet profound, lessons you’ll learn in dental school that will stick with you forever.
- The power of a friendly smile
It’s often said that a smile is the universal language of kindness, and you’ll quickly realise that as a dental student, your smile can go a long way. Whether you’re introducing yourself to a nervous patient or comforting a peer, the impact of a simple, warm smile cannot be overstated.
You might not have been taught this in lectures, but you’ll soon discover that a smile can break down barriers and make your clinical environment more welcoming. Plus, learning to put patients at ease with just your expression can be just as crucial as knowing the latest dental techniques.
- Dental tools are like your ‘instruments of magic’
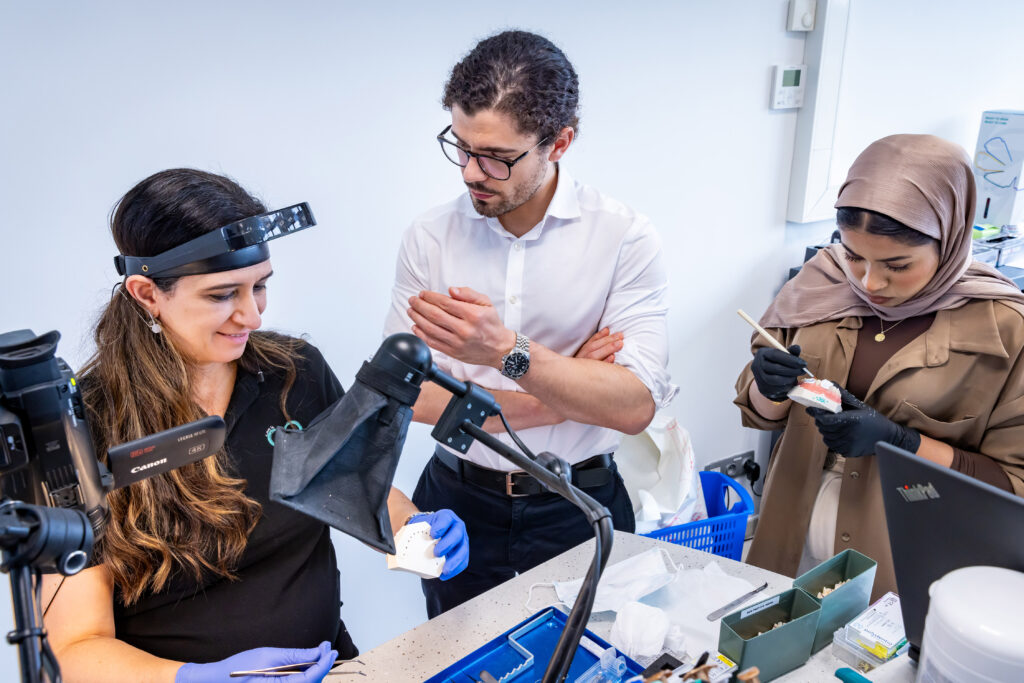
When you first start dental school, you might look at your instruments with a sense of curiosity. Over time, however, these tools become extensions of yourself. Your mirror, explorer, and scalers will feel like trusted companions, and you’ll develop a surprising fondness for them.
This hands-on experience teaches you not just the technicalities but the artistry of dentistry. Whether it’s the precise angle of your hand while scaling or the delicate touch needed to fill a cavity perfectly, you’ll learn that every instrument in your hand plays an important role in creating a patient’s smile. It’s almost like you’re a wizard in a very precise world of magic.
- You’ll become a master of time management (even if you don’t want to)
Dental school doesn’t just teach you how to become a dentist; it teaches you how to juggle. Managing your time between classes, clinical sessions, assignments, and social activities (yes, there is time for those too) will become second nature to you.
It won’t always be easy – some days you’ll feel like there aren’t enough hours in the day – but you’ll become incredibly skilled at planning, prioritising, and making the most of your time. In fact, you’ll soon find yourself scheduling breaks to keep your sanity and realise that time management is key to surviving dental school and life after graduation.
- You’ll learn how to tell ‘bad news’ with compassion (and a smile)
One of the most underrated lessons you’ll learn in dental school is how to break difficult news to patients. Whether it’s informing them that they need a root canal, their wisdom teeth need to be removed, or they have an unexpected diagnosis, this is a skill you’ll develop over time.
What you weren’t likely taught in lectures, though, is how to deliver the news with empathy and kindness. Communication skills will evolve as you learn to balance the technical aspects of dentistry with emotional intelligence. It’s a delicate skill that will stay with you for the rest of your career, helping you build lasting trust with your patients.
- You’ll develop a love for the little things
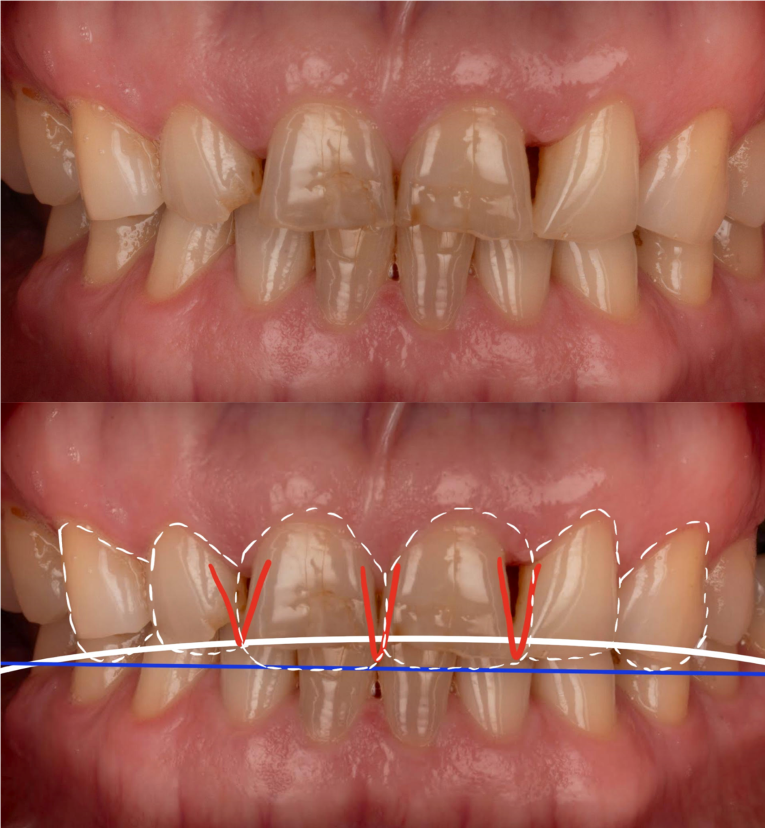
While dental school is often associated with heavy textbooks and complex clinical procedures, you’ll quickly learn to appreciate the smaller details of the profession. From the way a perfectly moulded crown fits snugly to the satisfaction of a beautifully contoured filling, these subtle moments will become your favourite parts of the job.
It’s in these little things – like perfectly polished teeth or the joy of seeing a nervous patient leave your office smiling – that you’ll truly begin to appreciate the artistry and impact of dentistry.
- You’ll learn to adapt (a lot)
No two days in dental school are the same, and this is a lesson that will come to you quickly. Whether you’re dealing with a change in schedule, a new procedure, or a challenging patient, you’ll need to learn to think on your feet and adapt to new situations.
You won’t always have the luxury of following a textbook, but you will develop an ability to think critically, solve problems in real-time, and adapt your approach when necessary. This adaptability will become one of your greatest assets as you transition into the fast-paced world of dentistry.
Conclusion: dentistry is an art and a science, but it’s also a journey of self-discovery
While dental school undoubtedly challenges you academically and professionally, it’s also a time for personal growth and discovery. The unexpected lessons – whether it’s learning how to calm a nervous patient with a smile or realising that your instruments are your trusted allies – will stick with you for the rest of your career.
Remember, dentistry isn’t just about the knowledge you gain from textbooks; it’s also about the experiences, the people, and the moments that shape you into a compassionate, skilled professional. So, embrace these quirky lessons along the way, because they are the ones that will make you not just a great dentist but a great human being.
Author bio
“I am a third-year dental student at the University of Bristol, with a particular interest in restorative and aesthetic dentistry. I am especially passionate about the subtle artistry involved in restoring not only smiles but also confidence and wellbeing. As I progress through my studies, I am increasingly fascinated by the way dentistry blends scientific precision with empathy and creativity – a balance I hope to carry forward into my future career.
Away from the dental clinic, I find inspiration in quiet moments: long walks, a good matcha, and the timeless comfort of literature, particularly poetry. One piece I often return to is If— by Rudyard Kipling, a powerful reminder of resilience, self-mastery, and integrity, qualities I believe are just as vital in dentistry as they are in life. Much like in dentistry, it is often the smallest, most thoughtful details that leave the greatest impact.”
Sana Masood

Sign up to our monthly newsletter
Follow us on social media: