The College has announced the topic and speakers for its next annual study day in Glasgow.

Delivering lectures under the title “Digital dentistry for the dental team: you say you want a revolution” will be four speakers: Dr Noland Naidoo, Dr Helen Kaney FCGDent, Professor Murali Srinivasan and Professor Gerry McKenna FCGDent.
The annual study day, organised by CGDent Scotland, takes place at Glasgow Science Centre on the first Friday in December – 4 December this year. With six hours of CPD, the day is attended by up to 400 dental professionals from across the UK, and finishes with a drinks reception which marks the start of the festive season for its many regular attendees.
Dr Noland Naidoo is a specialist prosthodontist who practises prosthodontics and endodontics in Edinburgh and Kelso, and previously co-led a private prosthodontic practice in Johannesburg. He qualified BChD from the University of the Western Cape in 2005, and was awarded a PDipDent in Implantology two years later before completing his MDent in Prosthodontics at the University of the Witwatersrand, where he later became a specialist in the Department of Oral Rehabilitation. He relocated to the UK in 2022, joining University College London’s Eastman Dental Institute as a clinical lecturer on postgraduate prosthodontic programmes, and then to Edinburgh in 2024, where in addition to his practice he has taught on postgraduate prosthodontic and endodontic programmes at Edinburgh Dental Institute. He is a Fellow of the International Team for Implantology (ITI), an alumnus of Future Leaders in Prosthodontics (FLiP) and serves on the board of the Shaping the Future of Implant Dentistry (SHIFT) leadership programme. He has contributed to international professional organisations, including the International College of Prosthodontists, and acts as a peer reviewer for leading journals.
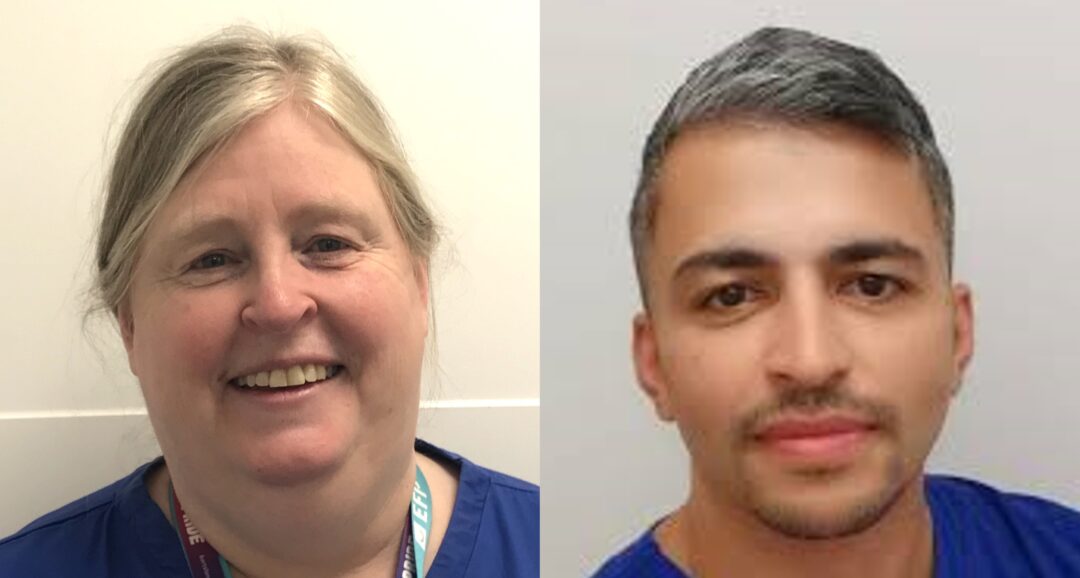
Dr Helen Kaney FCGDent is Head of the Dental Division at the Medical and Dental Defence Union of Scotland (MDDUS). She qualified BDS from Glasgow University in 1987 and spent many years in general dental practice as well as working as a clinical assistant in conservative dentistry and prosthodontics at Glasgow Dental Hospital and at Guy’s Hospital in London. She developed an interest in law and ethics early in her career before training and working as a solicitor for a number of years, acting for doctors and dentists in clinical negligence claims, regulatory matters and Fatal Accident Inquiries in Scotland on the instructions of UK indemnity providers. Her first dentolegal role started in 1999, working for a large insurer in Surrey, and she has since accrued significant experience in advising and assisting dentists in the UK and Ireland and in several other jurisdictions, including during 14 years working for Dental Protection, latterly as Head of Dental Services in Scotland. She holds a Bachelor of Laws (LLB) and a Diploma in Legal Practice, and completed an MBA at Strathclyde Business School in 2013. A Fellow of the College of General Dentistry, she was an elected member of its Council from 2019-25.
Professor Murali Srinivasan is a specialist prosthodontist, Director of the Clinic of General, Special Care and Geriatric Dentistry at the University of Zurich and an honorary professor at Chulalongkorn University in Bangkok. He is a past President of the European College of Gerodontology, former Head of the University of Zurich’s Centre for Dental Medicine, and is currently President of both the International Association of Dental Research’s Geriatric Oral Research Group (IADR-GORG) and the Swiss Society of Gerodontology and Special Care Dentistry. He qualified BDS in India in 1996, completed his Master of Dental Surgery in prosthodontics in 2001 and also holds both a Master of Advanced Studies in reconstructive dentistry and a Doctorate in Dental Medicine from the University of Geneva. Formerly practising in Dubai, he moved to Switzerland in 2011 on an ITI scholarship, after which he became a Lecturer, later Senior Lecturer, at the University of Geneva. An active Fellow of the ITI, he has published numerous papers in peer-reviewed journals. His current research encompasses implant dentistry, geriatric dentistry, prevention and the clinical applications of CAD-CAM technology in removable prosthodontics.
Professor Gerry McKenna FCGDent is a Consultant in Prosthodontics and Restorative Dentistry at Queen’s University Belfast, where his clinical work is focused on fixed and removable prosthodontics, including managing older adults in both hospital and private practice. He also leads oral health research within the university’s Centre for Public Health, focussing on optimising treatment options for older adults. After qualifying BDS from Newcastle University in 2004, he worked in a number of dental hospitals, spent time in dental practice, achieved a PhD on the impact of a tailored dietary intervention coupled with oral rehabilitation on the nutritional status of older adults, and completed specialist clinical training at University College Cork. A Vice President of IADR-GORG and past President of both the IADR’s Irish Division of and the European College of Gerodontology, he is an adjunct Professor at University College Cork, King James IV Professor at the Royal College of Surgeons of Edinburgh, and a Fellow of both the College of General Dentistry and RCS Edinburgh. He has recently published the book Clinical Cases in Gerodontology.
The CGDent Scotland Study Day is open to all dental professionals, and can be attended in person or virtually.
Fee discounts are available to College members as follows: College dentist members can buy their tickets for just £149 (£249 once ‘early bird’ places are sold out), compared to the full rate for non-member dentists of £349. The concessionary rate for dental technicians, dental hygienists, dental therapists, dental nurses, practice managers and retired practitioners is £149, but for College members in these categories it is just £129.
Breakfast rolls, a two-course lunch, refreshments throughout the day and evening drinks are all included in the attendance fee, and there will be an accompanying trade exhibition to visit.

Professor Jim McCaul, lead maxillofacial surgeon at the Queen Elizabeth University Hospital in Glasgow, delivering his lecture, ‘Oral Cancer, what you need to know and what you need to do’, to attendees at last year’s CGDent Scotland Study Day
Other discounts to the full rate are available to Foundation Dentists / Vocational Trainees and their trainers, recent graduates and members of the Glasgow Odontological Society and the Royal Odonto-Chirurgical Society of Scotland.
For further information, visit our events pages.
A review of the CGDent Scotland 2025 Study Day is available here