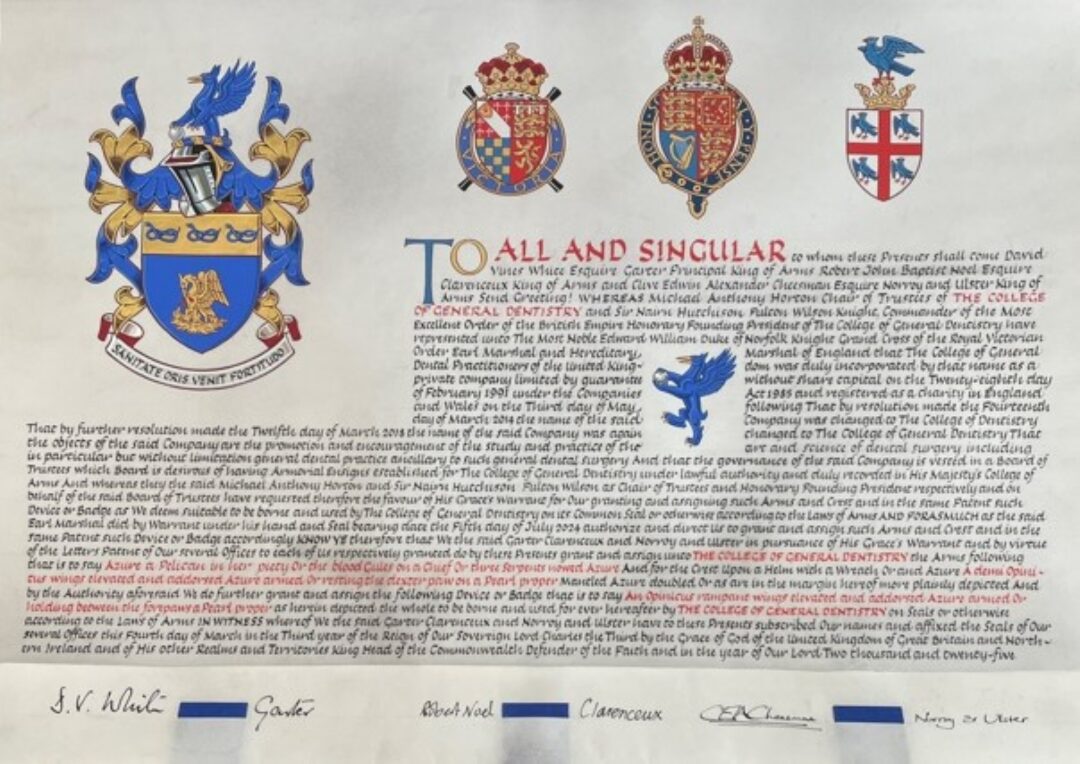
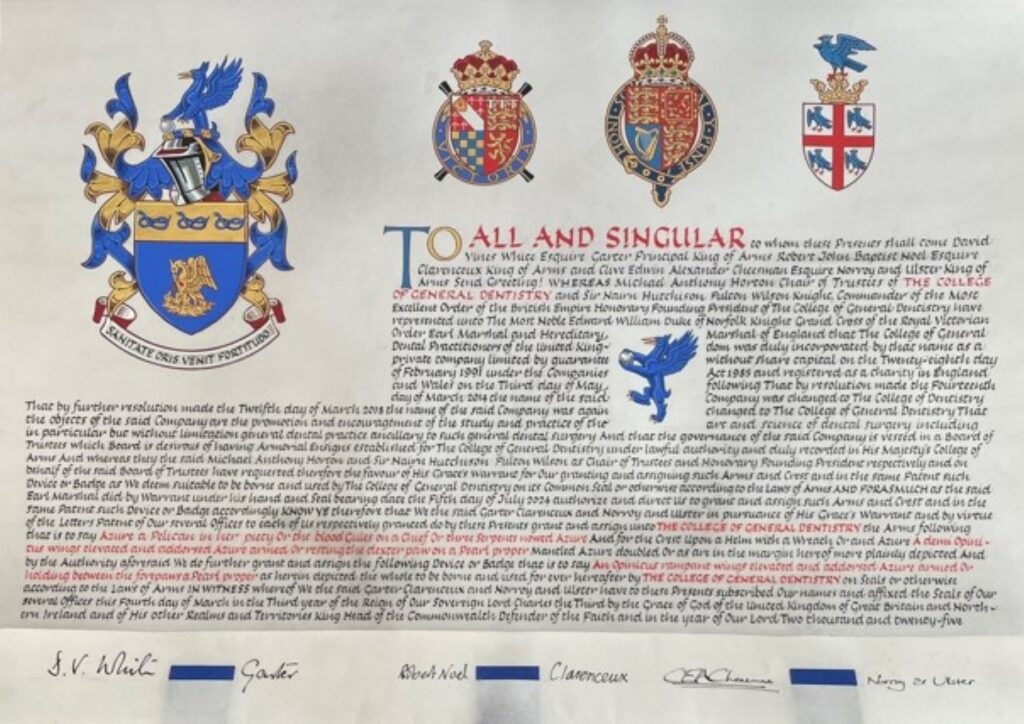
The College has published the full text of its recently-received Grant of Arms.

The Grant of Arms to the College – as reported here – was authorised in July 2024, signed in March 2025 and received in May 2025. The text of the Grant is as follows:
TO ALL AND SINGULAR to whom these Presents shall come David Vines White Esquire Garter Principal King of Arms Timothy Hugh Stewart Duke Esquire Clarenceux King of Arms and Robert John Baptist Noel Esquire Norroy and Ulster King of Arms Send Greeting! Whereas Michael Anthony Horton Chair of Trustees of The College of General Dentistry and Sir Nairn Hutchinson Fulton Wilson Knight, Commander of the Most Excellent Order of The British Empire Honorary Founding President of The College of General Dentistry have represented unto The Most Noble Edward William Duke of Norfolk Knight Grand Cross of the Royal Victorian Order Earl Marshal and Hereditary Marshal of England that The College of General Dental Practitioners of the United Kingdom was duly incorporated by that name as a private company limited by guarantee without share capital on the Twenty-eighth day of February 1991 under the Companies Act 1985 and registered as a charity in England and Wales on the Third day of May following That by resolution made the Fourteenth day of March 2014 the name of the said Company was changed to The College of Dentistry That by further resolution made the Twelfth day of March 2018 the name of the said Company was again changed to The College of General Dentistry That the objects of the said Company are the promotion and encouragement of the study and practice of the art and science of dental surgery including in particular but without limitation general dental practice ancillary to such general dental surgery And that the governance of the said Company is vested in a Board of Trustees which Board is desirous of having Armorial Ensigns established for The College of General Dentistry under lawful authority and duly recorded in His Majesty’s College of Arms And whereas they the said Michael Anthony Horton and Sir Nairn Hutchinson Fulton Wilson as Chair of Trustees and Honorary Founding President respectively and on behalf of the said Board of Trustees have requested therefore the favour of His Grace’s Warrant for Our granting and assigning such Arms and Crest and in the same Patent such Device or Badge as We deem suitable to be borne and used by The College of General Dentistry on its Common Seal or otherwise according to the Laws of Arms And forasmuch as the said Earl Marshal did by Warrant under his hand and Seal bearing date the Fifth day of July 2024 authorize and direct Us to grant and assign such Arms and Crest and in the same Patent such Device or Badge accordingly Know Ye therefore that We the said Garter Clarenceux and Norroy and Ulster in pursuance of His Grace’s Warrant and by virtue of the Letters Patent of Our several Offices granted by Her late Majesty to each of Us respectively do by these Presents grant and assign unto The College of General Dentistry the Arms following that is to say: Azure a Pelican in her piety Or vulning herself Gules on a Chief Or three Serpents nowed Azure And for the Crest Upon a Helm with a Wreath Or and Azure A demi Opinicus wings elevated and addorsed Azure armed Or resting the dexter paw on a Pearl proper Mantled Azure doubled Or as are in the margin hereof more plainly depicted And by the Authority aforesaid We do further grant and assign the following Device or Badge that is to say: An Opinicus rampant wings elevated and addorsed Azure armed Or holding between the forepaws a Pearl proper as herein depicted the whole to be borne and used for ever hereafter by The College of General Dentistry on Seals or otherwise according to the Laws of Arms In witness whereof We the said Garter Clarenceux and Norroy and Ulster have to these Presents subscribed Our names and affixed the Seals of Our several Offices this Fourth day of March in the Third year of the Reign of Our Sovereign Lord Charles the Third by the Grace of God of the United Kingdom of Great Britain and Northern Ireland and of His other Realms and Territories King Head of the Commonwealth Defender of the Faith and in the year of Our Lord Two thousand and twenty-five. |
Details of the historical and professional significance of each element of the College’s distinctive Coat of Arms, as described in and visible on the Grant, are available here.
The Grant was on display at the College’s Summer Reception which took place on Friday 13 June 2025 in Sheffield.
This article was updated on 9 July 2025 to provide a link to the description of the heraldry behind the design of the College’s Coat of Arms, and to update the section referring to the display at the College Summer Reception.