Abhi Pal, President of the College of General Dentistry, says action by dental teams to promote understanding of oral cancer, antimicrobial resistance and the perils of excess sugar consumption can help reduce the burden of disease and prevent premature death.
Of the many significant causes which our College of dental professionals supports, it so happens that three of those around which annual campaigns are organised fall in November.
Mouth Cancer Action Month, organised by the Oral Health Foundation, raises public awareness of oral cancer, highlights the risk factors, educates people on what to look for and how to self-check, and encourages those who see anything unusual to visit their dental practice as soon as possible.[i]
Despite this vital work, the incidence of oral cancer has risen by 97% in the UK over the last 20 years, driven by a variety of lifestyle factors such as tobacco use and alcohol consumption.[ii]
Another of the causes is a rise in infection with human papillomavirus (HPV), which causes 5% of all cancers and is the leading cause of oropharyngeal cancers. Over two-thirds of oral cancer diagnoses are in men [iii], and those who were members of the Faculty of General Dental Practice UK (FGDP) should feel proud to be have been part of the successful HPV Action campaign – backed in a poll by 97% of FGDP and BDA members – for boys to be offered vaccination against HPV (just as girls have been since 2008), which will offer protection to 400,000 young men each year once fully rolled out.[iv]
Public awareness of the major signs and symptoms of oral cancer is, however, as low as 23%, and diagnosis is often at a late stage, and the number of deaths is also rising.[v] But chances of survival are much improved if cancer is detected and treated early, and general dental practitioners are uniquely placed to highlight risky behaviours to patients, to check for signs of cancers of the head and neck during the routine examination, to make referrals where they suspect a patient may have cancer or a pre-cancerous lesion, and to reassure, support and encourage patients to attend their referral appointment.
Dental practices can also play an important preventative role by raising awareness and displaying information in waiting areas, and crucially help ensure speedy access to treatment if needed by knowing their local referral pathway in advance.
CGDent’s new oral cancer webpage highlights guidelines, recommendations, webinars, posters and other resources which can help general dental teams play their part in tempering the rise in oral cancer, and I encourage you to take a look and bring it to the attention of practice colleagues.
World Antimicrobial Awareness Week, instigated by the World Health Organisation, runs from 18-24 November each year, starting with European Antibiotic Awareness Day on 18th.[vi] Antimicrobial resistance (AMR) is a global problem that leads to antibiotics no longer being effective in treating even simple infections, and there are serious consequences for everyone, particularly those undergoing major surgery, chemotherapy, organ or stem cell transplants.
Public discussion on this subject can sometimes give the impression that this is an issue for future generations to worry about, perhaps even a hypothetical one, but the scale of the problem is already significant. More than 2.8 million antibiotic-resistant infections occur in the US each year, and more than 35,000 people die as a result.[vii] And every year 25,000 people across Europe, and 700,000 worldwide, die from antibiotic-resistant infections, and it has been estimated that the annual global toll could be as high as 10 million by 2050.[viii]
Dentists issue around 5-7% of all antibiotic prescriptions in the NHS, and dental teams have a vital role to play in keeping antibiotics working by prescribing them only when necessary, and by educating patients to take and dispose of them responsibly.
It is a requirement of all healthcare providers in England that “procedures should be in place to ensure prudent prescribing and antimicrobial stewardship. There should be an ongoing programme of audit, revision and update” [ix], and these are good principles to follow regardless of where you practise.
Three key resources which can help you to do so were co-developed by the FGDP, and are now published by the College via our Standards & Guidance homepage:
- The Antimicrobial Prescribing Self-Audit Tool helps dental prescribers to complete a clinical audit of their antimicrobial prescribing and management of dental infections, and to compare audited practice against the guidance
For many years the Faculty, together with the Association of Clinical Oral Microbiologists (ACOM), co-ordinated a collaboration of organisations to promote stewardship of antimicrobials, and this year the College picked up the Faculty’s role, working with ACOM to bring together 11 organisations across medicine and dentistry to hammer home the message that ‘antibiotics don’t cure toothache’.
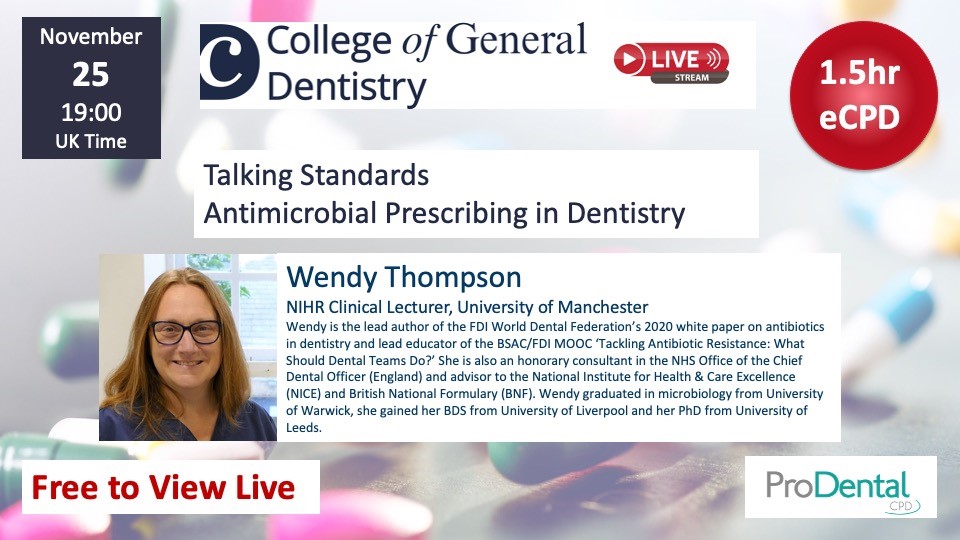
Last year, our AMR Lead, Dr Wendy Thompson, presented a webinar on this theme called Now the drugs won’t work – treating people with toothache. Tonight she also led a new webinar called Talking standards: Antimicrobial prescribing in dentistry, offering a refresher on the guidelines, exploring how dental teams can help keep patients safe from untreatable infections, considering why dental practitioners might overprescribe antibiotics, and discussing the impact of COVID-19 on prescribing rates. We also heard powerful testimony from Vanessa Carter, a survivor of a multi-drug-resistant strain of MRSA, and member of the WHO Strategic Technical Advisory Group on antimicrobial resistance, which really illustrated the importance of antimicrobial stewardship, and I would commend you to watch. Co-produced with our CPD partner, ProDental, both recordings are available to CGDent members free of charge using the links above.
Sugar Awareness Week, organised by Action on Sugar from 8-14 November, aims to raise public awareness of the poor health outcomes associated with excess sugar consumption, and to get people talking about the importance of sugar reduction.[x]
The College of General Dentistry’s support continues that previously given by the FGDP, and the two organisations were among those who successfully campaigned for a ‘sugar tax’ on soft drinks, which since its introduction in 2016 has seen a 29% reduction in the sugar content of drinks subject to the tax, and a shift in purchasing towards lower sugar alternatives.[xi] We have also been pleased to see the further restrictions on the advertising and promotion of high sugar items which are starting to take place, and hope this will continue.
Action on Sugar’s analyses of the sugar content of individual food products and product categories frequently provide the substance behind extensive media coverage of this issue that you will have seen in recent years, and this year’s campaign focussed on the high sugar content often seen in snack foods marketed as healthy, and also called for the removal of misleading sugar claims on sweet baby and toddler snacks such as biscuits and rusks.
As a dental organisation, the College works with Action on Sugar to highlight the association between sugar consumption and poor oral health. As dental teams know all too well, tooth decay, despite being almost wholly preventable, affects around a quarter of 5-year-olds [xii], a third of 12-year-olds and almost half of 15-year-olds [xiii], and tooth extraction is the number one reason young children are admitted to hospital [xiv]. Reducing sugar intake also lowers our risk of a wide range of illnesses including obesity, type 2 diabetes, heart disease, stroke – and indirectly of some cancers.
My sense is that public understanding of these links has been growing for some time, yet as a nation we consume three times the amount of sugar we should be [xv]. The scale of the challenge to produce a decisive shift in behaviour therefore remains daunting, but dental practices have long been at the forefront of promoting reduced sugar consumption. To complement the messages delivered during clinical appointments, I would encourage practices to browse the many resources available on Action on Sugar’s website (http://www.actiononsugar.org/) and consider displaying its posters in their waiting area.
You may also be interested to watch the webinar recording Helping Our Patients to Kick Sugar, presented by London dentist and author of the ‘Kick Sugar’ cookbook, James Goolnik. As above, this is available free of charge to College members and comes with CPD hours.
As a member of the FGDP for almost a quarter of a century, I was extremely proud of its consistent work promoting action to tackle oral cancer, antimicrobial resistance and the overconsumption of sugar, and as President of the College of General Dentistry I am delighted to say that we are picking up where the Faculty left off.
Attracting and sustaining the public’s attention is very difficult. Raising awareness, changing perceptions, and advocating for change to the point that action is seen by decision makers as both necessary and likely to receive popular support, is often the work of decades. But it can and has been done in many areas, starting with a small army of committed advocates spreading the word at every opportunity, eventually leading to widespread understanding and support among the public, the media and politicians.
So while these three campaigns run each November, general dental practice teams can make a huge difference all year round, helping to promote a reduction in the burden of disease and premature death through their daily actions. These are issues which require our thought and conscientious action on a perennial basis – we must remember, remember.
[i] Mouth Cancer Action Month, Oral Health Foundation: https://www.dentalhealth.org/mouthcancer (accessed November 2021)
[ii] The State of Mouth Cancer UK Report 2020/21, Oral Health Foundation and Denplan (2021): https://www.dentalhealth.org/Handlers/Download.ashx?IDMF=33f0d4c5-aa47-4e06-9454-9914e2476614
[iii] Head and Neck Cancer statistics, Cancer Research UK: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers (accessed November 2021)
[iv] ‘’Decision to finally offer boys HPV vaccine will save many lives’: Declares charity’, Oral Health Foundation (2018): https://www.dentalhealth.org/news/decision-to-finally-offer-boys-hpv-vaccine-will-save-many-lives-declares-charity
[v] The State of Mouth Cancer UK Report 2020/21, Oral Health Foundation and Denplan (2021): https://www.dentalhealth.org/Handlers/Download.ashx?IDMF=33f0d4c5-aa47-4e06-9454-9914e2476614
[vi] World Antimicrobial Awareness Week, World Health Organisation: https://www.who.int/campaigns/world-antimicrobial-awareness-week/2021 (accessed November 2021)
[vii] Antibiotic Resistance Threats in the United States, 2019, Centers for Disease Control and Prevention (2019): https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
[viii] Tackling Drug-Resistant Infections Globally: Final Report and Recommendations, The Review on Antimicrobial Resistance (2016): https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
[ix] The Health and Social Care Act 2008 Code of Practice on the prevention and control of infections and related guidance, UK Department of Health (2015): https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/449049/Code_of_practice_280715_acc.pdf
[x] See http://www.actiononsugar.org/sugar-awareness-week/sugar-awareness-week-2021/get-involved/
[xi] Sugar reduction: Report on progress between 2015 and 2018, Public Health England (2019): https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/839756/Sugar_reduction_yr2_progress_report.pdf
[xii] ‘Tooth decay in 5-year-olds now increasing in some parts of England’, Faculty of Dental Surgery of the Royal College of Surgeons of England (2018): https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/phe-oral-health-2017/
[xiii] Child Dental Health Survey 2013, England, Wales and Northern Ireland, Health and Social Care Information Centre (2015): https://digital.nhs.uk/data-and-information/publications/statistical/children-s-dental-health-survey/child-dental-health-survey-2013-england-wales-and-northern-ireland
[xiv] ‘Every 10 minutes a child in England has a rotten tooth removed’, Public Health England (2018): https://www.gov.uk/government/news/every-10-minutes-a-child-in-england-has-a-rotten-tooth-removed
[xv] National Diet and Nutrition Survey: results from years 7 and 8 (combined), Public Health England and the Food Standards Agency (2018): https://www.gov.uk/government/statistics/ndns-results-from-years-7-and-8-combined
Sign up to our monthly newsletter