The College of General Dentistry and Faculty of Dental Surgery of the Royal College of Surgeons of England have co-published a chairside synopsis of Antimicrobial Prescribing in Dentistry: Good Practice Guidelines.
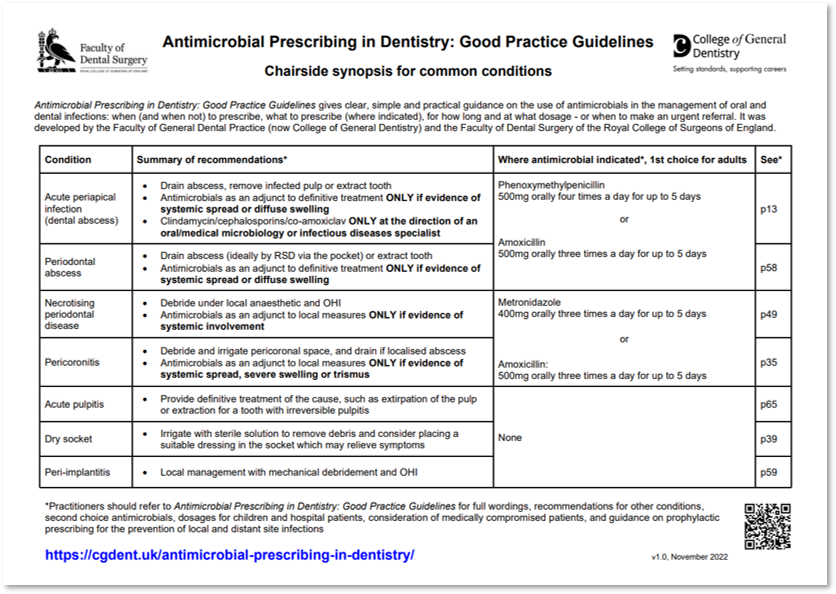
Antimicrobial Prescribing in Dentistry: Good Practice Guidelines offers clear, simple and practical guidance on the use of antimicrobials by dental teams, and the current third edition was developed by the Faculty of General Dental Practice (now College of General Dentistry) and the Faculty of Dental Surgery of the Royal College of Surgeons of England and published in 2020.
The new one-page synopsis summarises the recommended treatments for seven types of infection, including indications for the use of antimicrobials, and the first choice antimicrobial where use is indicated, with dosages and duration for adult patients.
Page references are indicated and a QR code included so that users can quickly and easily consult the appropriate section in the full guidance document, which also includes recommendations for other conditions, second choice antimicrobials (in case, for example, of penicillin allergy), dosages for children and hospital patients, consideration of medically compromised patients, and guidance on prophylactic prescribing for the prevention of local and distant site infections.
Dr Wendy Thompson PhD FCGDent, the College of General Dentistry’s lead on antimicrobial prescribing and stewardship, and the lead developer of the synopsis, said:
“The scale of the problem of antibiotic-resistant bacterial infections cannot be overstated. They already kill more people worldwide than HIV and malaria combined, and they will cause more deaths than cancer within a generation.
“By prescribing antibiotics only when strictly necessary, dental practitioners can keep antibiotics working and ultimately save lives. Using the new synopsis as an aide memoire, and referring to the full guidelines as necessary, will help them to do so.”
Mr Matthew Garrett, Dean of the Faculty of Dental Surgery of the Royal College of Surgeons of England, said:
“Our new one-page synopsis outlines treatment recommendations for a number of infections commonly encountered by dental practitioners, and makes it easy to access the full, detailed, condition-by-condition guidelines document, which is freely available online for the benefit of all dental professionals and their patients.
“If you only have time for one thing this World Antimicrobial Awareness Week, download and print out the new synopsis to help you play your part in combatting antimicrobial resistance all year round.”
Antimicrobial Prescribing in Dentistry: Good Practice Guidelines is available to view online free of charge, and College members can download it to access save, search and print functionality.
The new one-page synopsis is available for all dental professionals to download and print free of charge.
Both can be found on our Standards & Guidance page